Campylobacter Infection
Causes and Transmission of Campylobacter Infection
Campylobacter infection, or campylobacteriosis, is one of the leading causes of foodborne illness in the United States. Campylobacter infections often present with symptoms similar to many gastrointestinal illnesses making clinical differentiation challenging. Accurate and timely diagnosis is essential to identify the true cause, guide appropriate treatment, and prevent the spread of infection.
Campylobacter Testing Solutions
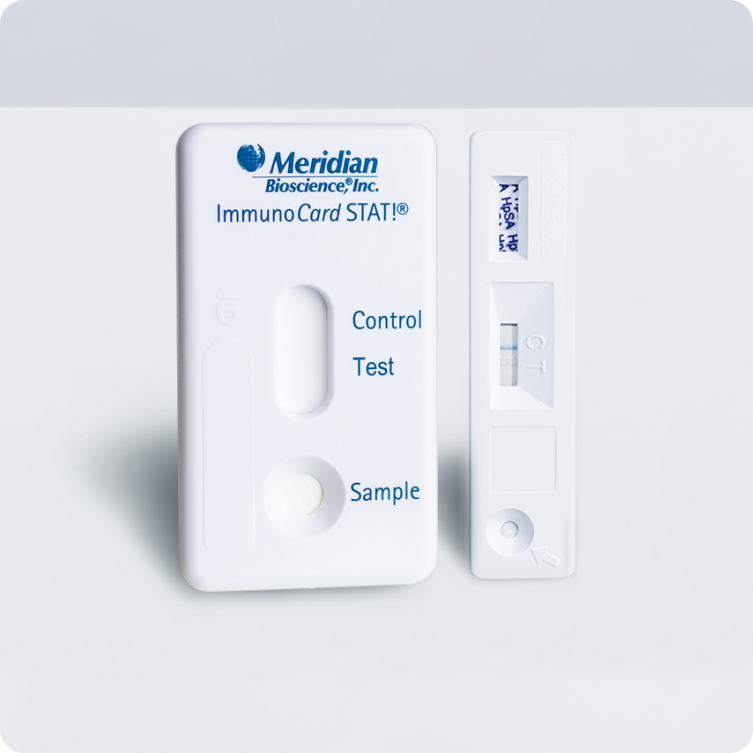
We provide advanced diagnostic solutions for Campylobacter infection—one of the leading causes of bacterial gastroenteritis worldwide. Powered by trusted technologies from Meridian Bioscience, including Curian® and Immunocard® STAT! Campy immunoassays, our solutions deliver rapid, accurate, and reliable detection of Campylobacter species from stool specimens.
Curian® Campy

Immunocard STAT!® CAMPY
Campylobacter Symptoms
Campylobacter symptoms typically manifest within two to five days after exposure to the bacteria and can include:
Diarrhea
Often watery or bloody, a common symptom of Campylobacter infection.
Abdominal Pain
Cramping or pain in the abdomen that may accompany diarrhea.
Fever
A moderate fever is commonly observed during infection.
Nausea & Vomiting
These symptoms can occur early in the infection phase.
These symptoms usually last about a week. While most recover without treatment, some may develop complications such as irritable bowel syndrome, arthritis, or Guillain-Barré syndrome—a rare neurological condition causing muscle weakness and paralysis.
Treatment of Campylobacter Infection
Most Campylobacter infections are self-limiting and resolve without the need for antibiotics. Supportive care, including staying hydrated and resting, is usually sufficient. However, antibiotics may be prescribed in severe cases or for patients at higher risk of complications.
FAQs
What is Campylobacter?
Campylobacter is a genus of bacteria that is one of the most common causes of foodborne illness. The most common species is Campylobacter jejuni, followed by Campylobacter coli, Campylobacter upsaliensis and Campylobacter lari.
How do people get infected with Campylobacter ?
Campylobacter infection is commonly contracted through the consumption of undercooked poultry, unpasteurized milk, contaminated water, or contact with infected animals.
What are the symptoms of Campylobacter infection?
Symptoms include diarrhea (often bloody), abdominal cramps, fever, nausea, and vomiting.
How is Campylobacter infection diagnosed?
Diagnosis is usually confirmed by testing a stool sample for the presence of Camplyobacter bacteria. Sometimes, additional confirmatory testing may be conducted to identify specific species.
How can Campylobacter infection be prevented?
Preventive measures include proper cooking of poultry, avoiding unpasteurized milk, practicing good hygiene, and preventing cross-contamination in the kitchen.
